"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
Date of admission 4th feb 2022
45yrs old female ,farmer by occupation , resident of nalgonda came to casuality with the Cheif complaints Of Fever and body pains not associated with chills, joint pains, cough and cold sore throat since 10days.
HOPI
Patient was apparently asymptomatic 10 days ago,then she developed fever which is sudden in onset and intermittent,not associated with chills, and has sore throat ,cough and cold which was relieved temporarily on medication.
The patient complains of joint pains( knee joint)since 5 years and generalised body pains and back ache since 10 days .
since 4 days she had an complain of dark coloured stools (melena).
She was found to be dengue positive patient. And was sent for treatment.
she complains of vomitings 1 episode 2 days back (night )which was non projectile.There is also an history of loss of appetite since yesterday.
There is no history of rashes, burning micturition,hematuria,hematemesis,no
Neck stiffness.
PAST HISTORY
There are no similar complaints in the past.
Not a known case of TB,HTN, Asthma, Diabetes, Epilepsy,CVA,CAD etc.
PERSONAL HISTORY
Diet-Mixed
Appetite-Normal
Bowel and Bladder movements-Regular
Sleep- adequate
## No Addictions
Medical history:-
Not allergic to any known drugs
Family history:-
No similar comolaints found in any of the family members
ON EXAMINATION
Patient was conscious, coherent, cooperative and we'll oriented to time,place and person
GENERAL PHYSICAL EXAMINATION
**Pallor- present
Icterus- absent
Cyanosis- absent
Clubbing- absent
Generalized lymphadenopathy- absent
**VITALS**
Temperature- 101.4F
Pulse rate -80bpm
Resp rate - 16cpm
Blood pressure-110/82mmHg
sPo2 98% at room temperature
SYSTEMIC EXAMINATION
CVS: Inspection
Chest wall is bilaterally symmetrical.
No precordial bulge is seen
Palpation
JVP- Normal
Apex beat -felt in the left 5th intercoastal space in the mid clavicular line
Auscaltation
S1&S2 are heard,no murmur found.
RESPIRATORY SYSTEM
Dyspnoea- no
No wheezing sounds
Position of trachea- central
Bilateral air entry, normal vesicular breath sounds are heard.
No added sounds
CNS
Patient is conscious
Speech normal
No signs of meningeal irritating
Motor and sensory system- Normal
Reflexes - present
Cranial nerves - intact
PER ABDOMEN
Liver non palpable
Spleen non palpable
Soft and Non tender.
FEVER CHART
04/02/22-06/02/22
INVESTIGATIONS
1st feb 222
##04/02/22
Hb-11.3
TLC-1500
Platelet count-42000
Rbs-242 & Fbs- 126
Hb1Ac-6.9
##05/02/22
Hb-11.6
TLC-2150
Platelet count-75000
USG
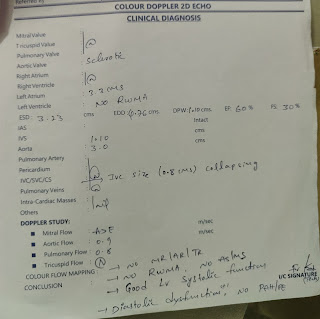
2D ECHO
PROVISIONAL DIAGNOSIS
VIRAL PYREXIA with thrombocytopenia
TREATMENT
IVF -NS,RL.DNS
Tab- paracetamol 650mg TID
Inj- PANTOP 40 mg
Inj- NEOMAL if temp rises above 102f
Inj-OPTINEURON 1mg Iv












Comments
Post a Comment